1) Lees A, Tapson K, Patel S. A qualitative evaluation of parents’ experiences of health literacy information about common childhood conditions. Self Care 2018;9(1)1-15.
This article reports the findings from a
qualitative service evaluation of health literacy resources for parents of
children aged 0-4 on six common paediatric conditions (abdominal pain,
asthma/wheeze, bronchiolitis, diarrhoea/vomiting, fever and head injury). These
have been launched across Wessex as part of the Healthier Together (HT) project
and consist of a website and paper-based resources designed to provide easily
accessible facts about common childhood conditions, advice on actions to take
in the event of certain symptoms and when and where to seek medical help.
Eighteen semi-structured interviews were conducted to investigate parents’
experiences of and reactions to the resources. We investigated perceived
effects on parental understandings and feelings about childhood illness and
help seeking behaviours. We discuss findings under four main headings: Parental
interaction with HT resources, Parents’ anxieties concerning their children’s
health, Positive evaluation and Areas for improvement. Parents positively
evaluated the aims of the project and the information provided. A small number
gave examples of resulting behaviour change and several anticipated future
changes. Parents expressed anxiety about childhood illness and making treatment
decisions. They required simple and easy to navigate resources including
prominent risk assessment information. Communication by health professionals
that reassures and empowers parents was also seen as important. Whilst this was
a small study we believe that the findings are of relevance to others
producing, disseminating and explaining health information aimed at parents and
other patient groups.
2) Fake E, Lees A, Tapson K, Patel S. Parental views on the management of young children with respiratory tract infections in primary care – a pilot study. Self Care 2018;9(4)23-34
BACKGROUND
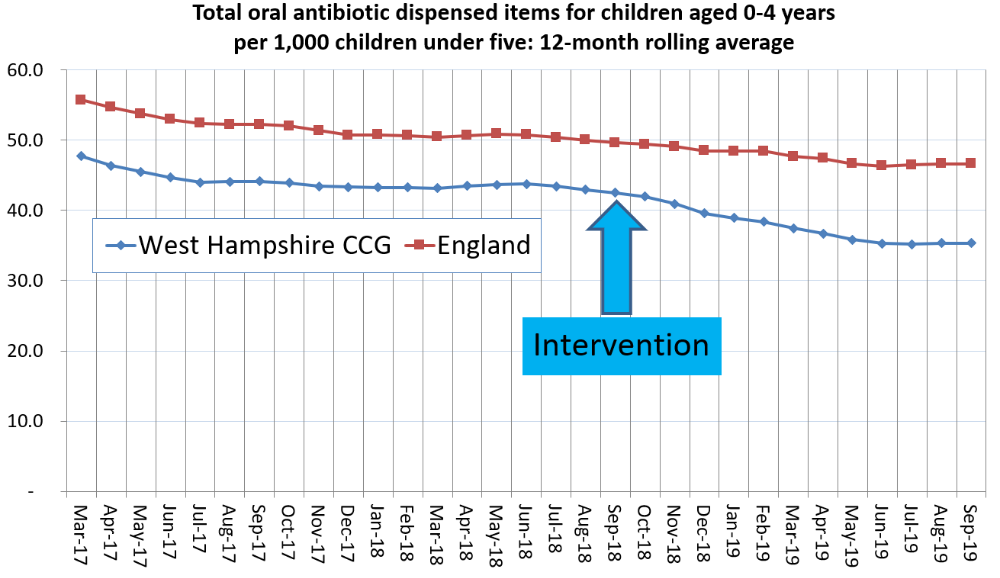
Local primary care data shows a 24% increase in the rate of acute
presentations with common self-limiting infections for children aged 0-4 years
between 2015/16 – 2016/17. As rates of serious illness have decreased, this
means increasing numbers of presentations could be managed elsewhere. Although
parents rarely expect antibiotics, they are often perceived to want them by
clinicians; potentially resulting in more antibiotic prescriptions and driving
future health-seeking behaviour.
AIMS
To explore parent expectations, concerns and opinions about the primary
care management of children presenting with respiratory tract infections
(RTIs).
METHODS
Semi-structured interviews with parents of children aged 0-4 years
presenting to primary care clinicians with symptoms of a respiratory tract
infection. Analysis involved thematic review
RESULTS
Parents used experience or ‘parental instinct’ when deciding to consult;
this was due to seeing a similar illness before and receiving treatment, or
alternatively having never seen this illness and being unsure of what to do.
Parents saw the usefulness of written information describing actions to take
and when to consult when their child was unwell. There was an about even split
between those preferring paper and those preferring web-based resources. All
parents sought input from a clinician for reassurance.
CONCLUSION
Better understanding of parent expectations when consulting clinicians
with unwell children could facilitate a more effective consultation. Parents
expect reassurance about their child’s illness, but inconsistent advice and
management from healthcare professionals, such as prescribing antibiotics, act
to increase parental anxiety and potentially drives future health-seeking
behaviour. Changing the way clinicians communicate, including the use of
consistent messages, may have a positive impact during current and future acute
illnesses.
3) Donovan E,
Wilcox CR, Patel S, Hay AD, Little P, Willcox ML. Digital interventions for
parents of acutely ill children and their treatment-seeking behaviour: a
systematic review. British Journal of General Practice 2020; 70 (692):
e172-e178.
Background Consultations for self-limiting
infections in children are increasing. It has been proposed that digital
technology could be used to enable parents’ decision making in terms of
self-care and treatment seeking.
Aim To evaluate the evidence that digital
interventions facilitate parents deciding whether to self-care or seek
treatment for acute illnesses in children.
Design and setting Systematic review of studies
undertaken worldwide.
Method Searches of MEDLINE and EMBASE were made
to identify studies (of any design) published between database inception and
January 2019 that assessed digital interventions for parents of children (from
any healthcare setting) with acute illnesses. The primary outcome of interest
was whether the use of digital interventions reduced the use of urgent care
services.
Results Three studies were included in the
review. They assessed two apps and one website: Children’s On-Call — a US
advice-only app; Should I See a Doctor? — a Dutch self-triage app for any acute
illness; and Strategy for Off-Site Rapid Triage (SORT) for Kids — a US
self-triage website for influenza-like illness. None of the studies involved
parents during intervention development and it was shown that many parents did
not find the two apps easy to use. The sensitivity of self-triage interventions
was 84% for Should I See a Doctor? compared with nurse triage, and 93.3% for
SORT for Kids compared with the need for emergency-department intervention;
however, both had lower specificity (74% and 13%, respectively). None of the
interventions demonstrated reduced use of urgent-care services.
Conclusion There is little evidence to support
the use of digital interventions to help parent and/or carers looking after
children with acute illness. Future research should involve parents during
intervention development, and adequately powered trials are needed to assess
the impact of such interventions on health services and the identification of
children who are seriously ill.
4) Patel S,
Hodgkinson T, Fowler R, Pryde K, Ward R. Integrating acute services for
children and young people across primary and secondary care. British Journal of
General Practice 2020; 70 (693): 158-159.
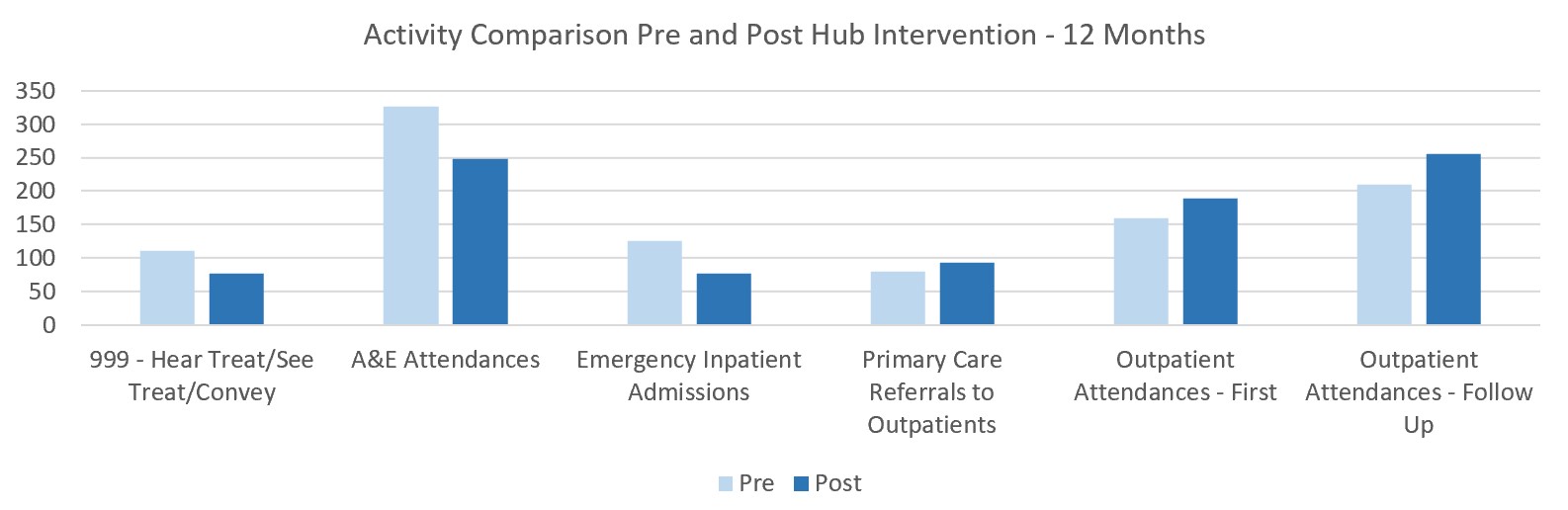
Children and young people under 18 years of age currently
account for approximately 25% of attendances to primary and secondary care but
only 12% of hospital admissions. The fact that children are the most likely age
group to attend emergency departments unnecessarily suggests that high levels
of parental anxiety is driving health seeking behaviour. This observation
justifies initiatives to deliver integrated acute services for CYP which
achieve consistency across primary and secondary care. Consistent management
and safety-netting by healthcare professionals reduces parental anxiety, which
in turn reduces urgent care presentations by empowering parents to confidently
self-manage minor illnesses. Addressing this avoidable activity would relieve
pressure on our currently overstretched urgent care services, improving access
and quality of care to those who need it most.